About the Procedure:
Oncoplastic Breast Surgery:
When a person is diagnosed with breast cancer, he or she will meet with a breast surgeon to determine the best treatment option. The breast surgeon is in charge of the cancer portion of the operation and will recommend either lumpectomy (removal of a portion of the breast) or mastectomy (removal of the entire breast). The appropriate surgical option and the decision regarding whether the nipple and areola can be saved during the surgery will depend on many factors, including location/size of the tumor, genetic predisposition for cancer, overall health, and the patient’s body habitus.
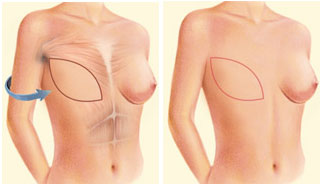
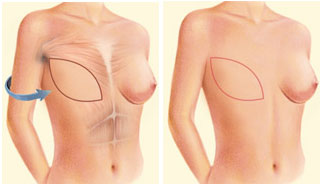
Lumpectomy is often used synonymously with breast-conserving surgery because a portion of the breast is removed and the remaining breast not affected by cancer is conserved. Radiation therapy often follows for treatment of the breast cancer. While lumpectomy can preserve a healthy amount of breast tissue, contour irregularities of the breast and other irregularities can develop from surgery and radiation therapy. These changes can create an abnormal breast shape and asymmetry between the breast affected by cancer and the opposite breast.
Women that have large or droopy breasts can benefit from a breast reduction/lift performed by a plastic surgeon at the time of lumpectomy. This collaborative oncoplastic surgery allows for treatment of cancer while optimizing the postsurgical size and shape of the breasts. On the day of surgery, Dr. Fischer designs special markings that the breast surgeon will use for a lumpectomy. Immediately following the lumpectomy, she will reduce and/or lift the breast affected by cancer, and perform a similar procedure on the opposite breast to create symmetry between the breasts. Please see Breast Lift (Mastopexy) and Breast Reduction procedure pages for more details.
Breast Reconstruction Following Mastectomy:
There are 3 main methods of reconstructing breasts following mastectomy. These include:
- Using tissue expanders and/or implants
- Using your own tissue (autologous tissue transfer)
- Using a combination of your own tissue (autologous tissue) with tissue expanders or implants
Tissue Expander/Implant-Based Breast Reconstruction:
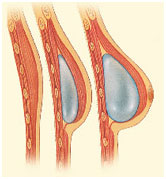
Tissue expander/implant-based breast reconstruction refers to using devices to recreate the breast. Sometimes reconstruction can be performed in a single stage; however, sometimes 2 stages are necessary to achieve the desired result. In a single-stage immediate reconstruction, a permanent implant is placed to recreate the breast at the time of mastectomy. All implants have a silicone shell and are either filled with silicone gel (silicone gel breast implant) or sterile salt water (saline breast implant). Sometimes a second surgery is necessary to enhance symmetry or to help correct contour irregularities from a mastectomy. If a second procedure is necessary, it is normally an outpatient procedure.
If an immediate 2-stage reconstruction is recommended, a tissue expander will be placed at the time of mastectomy. A tissue expander is a silicone shell that contains a magnetic metal port. The device is placed under your breast skin and is gradually filled with sterile salt water in the office following surgery. Most women report very minimal pain/discomfort during expansion. Expansion is complete when you are satisfied with the volume of your reconstructed breast. A second surgery is then performed to remove the tissue expander and place a permanent silicone gel or saline implant. The second surgery is normally performed under general anesthesia on an outpatient basis. Women report very little pain/downtime after the second surgery as the tissue expander has already created the space for the implant.
Sometimes an acellular dermal matrix is necessary to help support the tissue expander and/or implant during the reconstruction. Human acellular dermal matrix is skin (dermis) that is harvested from cadavers. The skin is then processed so that it is decellularized. The acellular dermal matrix serves as a scaffold to help support the tissue expander and/or implant. As time passes, your body incorporates the acellular dermal matrix into your own tissue. The acellular dermal matrix is not “rejected” by your body as kidney or liver transplants can be rejected because the matrix is decellularized.
Most patients stay in the hospital overnight for a 23-hour observation period. The recovery period is variable but many women take 4-6 weeks to return to work. You will be using your arms immediately after surgery for normal activities of daily living (eating, brushing teeth, etc.) but will be asked to avoid lifting > 5-10 lbs. with the affected arms for a few weeks after surgery.
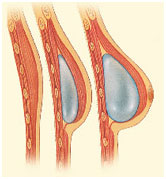
Image shows a side view of the chest.
Left: Ribs, pectoralis major muscle, and skin following mastectomy
Center: Partially filled tissue expander placed under the pectoralis major (chest muscle).
Right: Tissue expander fully inflated.
Using Your Own Tissue (Autologous Tissue Transfer):
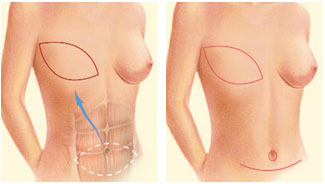
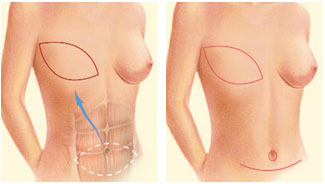
Breast reconstruction can be performed by transferring tissue from another area of your body to your chest. Common sites for obtaining tissue include your abdomen, inner thighs, and buttocks. During this procedure, the excess skin and fat from one of the aforementioned areas is taken away from your body and small blood vessels are reattached under a microscope to allow the tissue to survive. This procedure, called a free flap, recreates a breast without the use of tissue expanders and implants.
This form of reconstruction can be performed in an immediate or delayed fashion, meaning immediately following mastectomy, or weeks, months, or even years following mastectomy (delayed). The decision regarding the timing of reconstruction will depend on numerous factors and will be discussed with you during your consultation. If radiation therapy is necessary after mastectomy, it can be helpful to use a tissue expander as a place saver following mastectomy before proceeding with autologous tissue reconstruction. The tissue expander helps preserve the breast skin after surgery and during radiation therapy. Following radiation therapy, healthy tissue from the abdomen, inner thighs, or buttocks can be used to reconstruct the breast.
After length of stay in the hospital is 3-4 days following reconstruction with free tissue transfer. Recovery time is variable but can be slightly longer than implant-based reconstruction due to the additional operative site (abdomen, inner thigh, or buttocks).
Using a Combination of Your Own Tissue (Autologous Tissue) with Tissue Expanders or Implants:
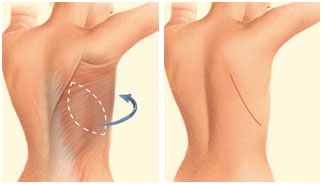
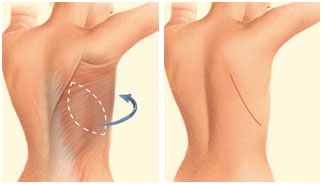
The latissimus dorsi muscle flap can be used to reconstruct a breast with or without the use of a tissue expander or implant. During this procedure, the breast is created by swinging skin, fat, and muscle from the back to the chest. To increase the volume of the back skin/fat/muscle, a tissue expander or implant can be placed underneath your own tissue. This form of reconstructing is often ideal if there is significant radiation skin damage to the chest because the radiated skin can be removed and replaced with healthy tissue from the back. Length of hospitalization after this form of reconstruction is typically 1-3 days with 4-6 weeks of recovery time.
Symmetry Procedures:
If a woman elects to have a mastectomy on the side affected by cancer, surgery can be performed on the other breast to achieve symmetry with the reconstructed breast. These symmetry procedures are a covered benefit under the Women’s Health and Cancer Rights Act (WHCRA) of 1998. Common procedures for symmetry include breast augmentation, breast lift (mastopexy), and breast reduction). If a women elects to have a mastectomy on the side affected by cancer, and a prophylactic (preventative) mastectomy on the opposite breast that is not affected by cancer, reconstruction can be performed on both breasts and is a covered benefit under WHCRA.
Nipple Areolar Complex Reconstruction:
If nipples/areolas are removed at the time of mastectomy or lumpectomy, reconstruction of the nipple areolar complex can be performed. Common modalities for nipple areolar complex reconstruction include 3-dimensional tattooing and local flaps of your own chest/breast skin to make a projecting nipple followed by tattooing for pigment. Nipple areolar complex reconstruction is normally the last procedure performed during a reconstruction.